About Treatment
Basal cell carcinoma is a slowly growing superficial papule or nodule that emerges from some cells in the epidermis. BCC is common malignant tumor among people of the white race, and every year the number of patients increases by 4-8%. It is observed in relation to other skin cancers, and its main reason is an increase in the ultraviolet load on the body, due to both social and natural factors.
BCC develops from epidermal stem cells or hair follicle progenitor cells.
The main signs of basal cell carcinoma are:
formation of pink color, flat along the periphery and the presence of crusts in the center;
red spot or irritation in the face, neck, or hands;
open ulcer or erosion that does not heal within 4 weeks;
shiny nodule of pearlescent color.
Basal cell carcinoma can be of different morphological forms, which differ in location, clinical features and the stage of tumor aggressiveness:
nodular ulcerative;
piercing;
warty (papillary, exophytic);
nodular (large nodular);
pigmented;
sclerodermiform;
scar-atrophic;
flat superficial basalioma;
Spiegler's tumor ("turban" tumor, cylindroma).
BCC is a tumor with slow local destructive growth, as well as with a very low possibility of metastasis. Nevertheless, timely visit to a doctor and following recommendations will contribute to a quick recovery. Otherwise, basal cell carcinoma is difficult to treat and, in general, an untimely appeal to specialists can lead to a fatal end.
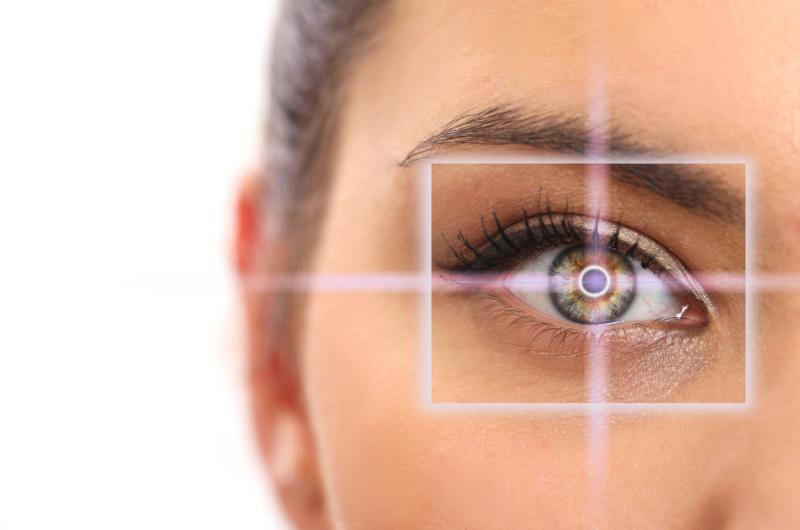
Basal cell skin cancer is diagnosed by dermatoscopy followed by tissue biopsy, as well as cytological or histological examination.
-
Risk Factors
Genetic predisposition and insolation play a role in the development of BCC.
Half of patients with BCC develop one or more new tumors over the next 3 years.
-
Complications
Complications of basal cell carcinoma can include:
Relapses
Increased risk of other types of skin cancer
The spread of cancer outside the skin
BCC treatment methods are divided into three main groups:
Surgical methods, which include:
Surgical excision of tumor is the main method of treatment for basal cell carcinoma. It is chosen most often because of the reliability and adequate margins of the resection, which is the basis for avoiding recurrence;
Curettage is less effective than surgical excision. Small indents from the edges of tumor lead to frequent relapses.
Minimally invasive methods:
Cryodestruction - destruction of tumor using liquid nitrogen. This technique has many disadvantages, in particular, scars, depigmentation, lack of histological material for further research. It should be noted that relapses occur in 30% of cases;
Laser excision of the tumor - used only for superficial spread of basal cell carcinoma. The main advantage is aesthetic component.
Conservative (non-surgical) methods:
Immunotherapy (treatment of tumor with antibodies);
Photodynamic therapy (the method is based on the use of photosensitizers and visible light of certain wave);
Radiation therapy (treatment with ionizing radiation);
Targeted therapy (blocks the growth of cancer cells by influencing the mechanism of action of specific target (targeted) molecules that are needed for carcinogenesis and tumor growth).
The choice of the treatment method depends on the location of the tumor, the development of the process and the presence of severe somatic pathology (especially in the elderly).
Based on statistics, the results of treatment for basal cell carcinoma are very satisfactory, but in any case, the result depends on the diagnosis and the start of treatment at the early stages of tumor development.
The frequency of control examinations is determined by attending physician.
Small BCCs in safe areas of the skin can be removed in a polyclinic with subsequent annual follow up (2 - 3 years).
Treatment and follow up of patients with BCC is carried out by an oncodermatologist. Multiple BCCs can be associated with rare hereditary diseases such as Gorlin syndrome.
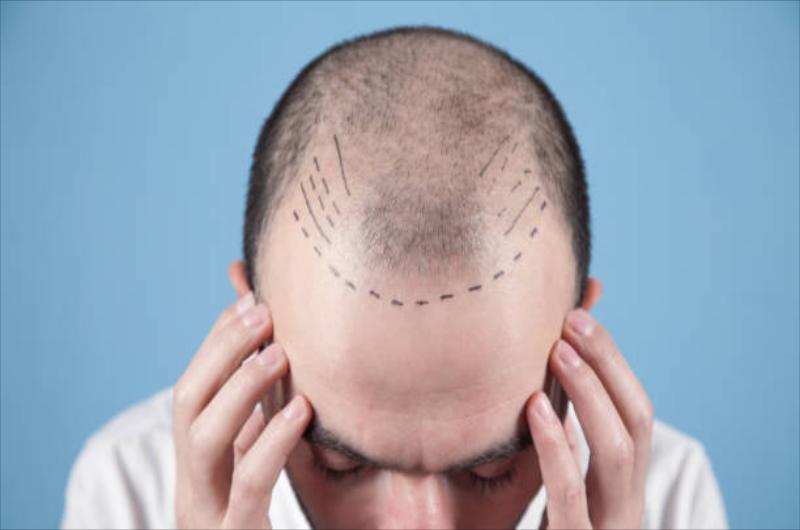
Basal cell carcinoma usually develops in areas of skin that are exposed to sunlight, especially the head and neck. Much less often, tumors of this type are found on the trunk and legs. However, basal cell carcinomas can develop on parts of the body that are rarely exposed to sunlight.
Although the first warning sign that may be a sign of basal cell carcinoma is an ulcer that does not heal or bleeds frequently, there may be other signs:
Pearly white or waxy mass on the skin, often containing blood vessels, located on the face, ears, or neck. Such formation can bleed, crusts can form. In dark-skinned people, the swelling may be brown or black.
Flat, scaly, brown or fleshy-looking spot on the back of the neck. Over time, such a spot can become quite large.
Less commonly, a white or waxy scar. This type of tumor is easy to miss, but it can be a sign of invasive and deforming basal cell carcinoma.
Basal cell carcinoma develops when mutations occur in the DNA of the basal cells. Basal cells lie at the bottom of the epidermis - the outer layer of the skin. New skin cells are formed from the basal cells. As new skin cells form, they push old cells to the surface of the skin, where old cells die and are shed.
The formation of new cells is controlled by the DNA of the basal cells. Mutation in DNA leads to rapid and abnormal divisions. Eventually, the accumulation of abnormal cell mass leads to tumor formation.
Ultraviolet radiation and other causes
The greatest damage to cell DNA comes from UV radiation from sunlight and artificial sources. However, exposure to UV rays does not explain the formation of carcinomas in areas that are not exposed to sunlight. This suggests that other factors may increase the risk of basal cell carcinoma, such as toxic substances or diseases of the immune system.