About Treatment
Liver cirrhosis is a pathology in which normal cells are replaced by scar tissue. This leads to the fact that the organ is unable to function normally. Toxins and bile accumulate in the liver, poisoning the entire body. In most cases, the disease is diagnosed in middle-aged Liver cirrhosis is a serious disease that requires severe and long-term treatment. However, the causes of this pathology can be completely different factors, many of which are amenable to, if not treatment, then control.
Characteristics and stages of development of liver cirrhosis
This lesion is the final stage of various chronic liver diseases. This diagnosis is made when pathological changes in the cells of an organ (hepatocytes) become irreversible. With cirrhosis, hepatocytes die as a result of the inflammatory process, and fibrous (connective) tissue forms in their place. In general, this process can be called immune-inflammatory. As a result, the structure of the liver is seriously damaged.
The destruction of hepatocytes is an extremely dangerous process, since these cells perform many important functions: they participate in metabolic processes and secretory activity (secretion of bile and processed substances into the intestine), neutralize toxins and other harmful substances. As a result, the liver ceases to perform its functions in full: harmful substances enter the circulatory system, causing intoxication of the body.
Liver cirrhosis has a staged course. Each stage differs in the degree of pathological changes, symptoms and necessary treatment.
The first stage has practically no symptoms, since the disease is compensated. Blood tests are characterized by a decrease in the level of bilirubin, as well as a decrease in the prothrombin index to 60–80 units. In this case, the inflammatory processes have already begun and the dead hepatocytes are replaced by connective tissue.
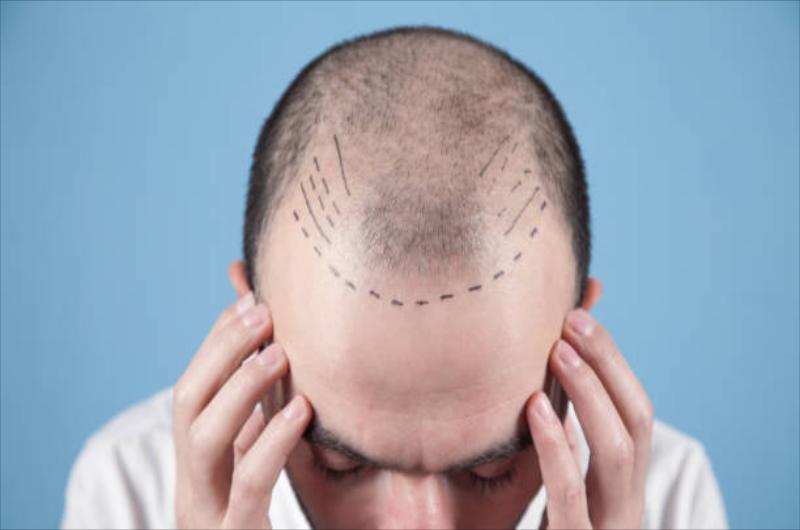
At the second stage of the disease, the first nonspecific symptoms begin to appear: weakness, apathy, headaches, nausea and diarrhea, poor appetite, discomfort in the right hypochondrium, nosebleeds and bleeding gums. In men, baldness and enlargement of the mammary glands are possible. Hepatic encephalopathy and ascites begin to appear. This stage is called subcompensated cirrhosis, since the disease can still be returned to the compensation stage.
This is followed by the terminal stage, at which encephalopathy and ascites progress, the skin becomes yellowish, muscle atrophy and anemia are observed. This stage is dangerous with the development of serious complications that can lead to death. These complications include hepatic coma, portal vein thrombosis, liver cancer, internal bleeding, and infectious complications.
Treament of Cirrhosis
Treatment of cirrhosis is a lengthy process, and it is not so much a treatment as a secondary prevention. At the same time, a special diet, hepatoprotective drugs and a complex of vitamins are prescribed, intake of hepatotoxic drugs, alcohol is excluded. In general, the formed cirrhosis of the liver is an irreversible condition and is considered incurable. Etiotropic therapy for most forms of liver cirrhosis is currently absent, with the exception of viral hepatitis, in which antiviral drugs can be prescribed.
Diet
With liver diseases, patients are usually prescribed diet, aimed at normalizing the functions of the organ and improving bile secretion. Food should be taken in small portions 5-6 times a day, while fried and fatty foods should be completely excluded. Preference should be given to boiled and steamed food. Be sure to drink enough water - at least 1.5 liters per day. You should completely avoid alcohol. The amount of protein is limited to a hundred grams per day, salt - 10 grams per day. With ascites, salt-free diet is prescribed.
Prohibited foods:
any chemical food additives, including canned food;
fried, salted, pickled, smoked;
confectionery, chocolate, ice cream;
animal fats, margarine, fatty meats and meat broth;
salty cheeses, dairy products with high fat content;
legumes, radish, spinach, radish, sorrel, garlic, onion;
sour fruits and berries;
sugary carbonated drinks, strong tea and coffee.
Homeopathic Medicines
However, one should not forget that homeopathy as such is not recognized by official evidence-based medicine, and its methods do not undergo serious clinical trials. Until now, there is no strong evidence that it works due to the declared beneficial components, and not due to the placebo effect. Not all homeopathic patients report an improvement in their well-being. In any case, homeopathic liver treatment is a long process, taking more than one month. The breakdown of hepatocytes and the growth of fibrous tissue can develop faster. If we talk about cirrhosis of the liver, then patient simply does not have time for risky treatment.
Drug Treatment
With compensated and subcompensated cirrhosis, supportive therapy is prescribed - a strict diet and hepatoprotectors (drugs based on glycyrrhizic acid, phospholipids, amino acids, milk thistle (Silybum marianum Carduus marianus) and other components that help restore liver function). Antiviral therapy (AVT) is used for viral cirrhosis. However, it is fair to say that there is no specific treatment for cirrhosis.
Surgical Intervention
If the above treatments do not help, liver transplant is performed. Surgical intervention is necessary at the last, decompensated, stage of the disease, when the liver no longer performs its functions. In addition, a part of the liver can be taken from a relative of patient or another person who has expressed his consent to this operation.
-
Causes
autoimmune disorders;
genetic disorders;
chronic cholestasis;
blockage of hepatic veins. -
Diagnostics
Blood tests (biochemical, for the presence of hepatitis);
Ultrasound of the abdominal cavity;
Gastroscopy;
CT;
Liver biopsy.
Cirrhosis can be caused by various reasons, and the most common of them is hepatitis viruses. Hepatitis C is the most dangerous for the liver, as it leads to the development of cirrhosis in 97% of cases. The alcoholic form develops as a result of the uncontrolled use of alcoholic beverages. The drug type occurs due to prolonged use of hepatotoxic drugs. The congenital form of cirrhosis is the result of some genetic pathologies (hemochromatosis, tyrosinosis, galactosemia, etc.). With insufficient blood circulation and prolonged venous stasis in the liver, a stagnant form of the disease is diagnosed. Alimentary cirrhosis develops as a result of metabolic disorders. Secondary biliary cirrhosis is a consequence of a violation of the outflow of bile. If the cause of the disease is not clear, such cirrhosis is called cryptogenic. Primary biliary cirrhosis also belongs to the category of diseases of unknown etiology.
The symptoms of liver cirrhosis depend on the stage of the disease. The main ones, regardless of etiology, are: reduced working capacity, unpleasant sensations in the abdomen, increased body temperature, joint pain. On examination, moderate increase in the spleen, increase and hardening of the liver, and deformation of its surface are revealed. In more serious stages, bloating, nausea and vomiting are observed, diarrhea is possible when eating fatty foods, heaviness and pain in the right hypochondrium. At the terminal stage, jaundice, ascites, leg edema, and varicose veins of the esophagus may occur. In some cases, hemorrhoids develop. If one or another liver disease is detected, it is necessary to consult a gastroenterologist-hepatologist
Preventive measures include any procedures to prevent hepatitis, which is a common cause of liver cirrhosis. It is recommended to lead a healthy lifestyle, give up alcohol and follow a balanced diet, not to get carried away with fried and fatty foods. Caution should be exercised when taking excessive medications, many of which are toxic to the liver. It is also worth taking care of leveling the unfavorable environmental conditions of the environment, which can have a negative effect on liver cells - take more rest in the fresh air.
One of the most effective methods of preventing cirrhosis is taking hepatoprotective drugs for liver diseases. They protect liver cells, restore their structure, reduce inflammation, normalize protein and lipid metabolism, and stop the development of fibrosis.
So, taking modern hepatoprotectors is a reliable and safe way to improve the clinical picture of liver disease, however, any self-medication is unacceptable, and, despite the fact that many drugs are approved for sale without a prescription, be sure to consult your doctor.