About Treatment
Interventional Gastroenterology
Interventional radiology in both treatment and diagnosis is one of the methods of minimally invasive medicine. It can be used for X-ray surgery and X-ray endovascular methods of treatment and diagnosis.
Any operation for a patient is a high risk of complications. Therefore, for a long time, specialists optimize complications such as bleeding, inflammatory changes, large scars and others. For about 30 years, a separate field of medicine has been developing, known as interventional radiology, which allows surgical intervention to be performed, that means, without a scalpel. It was first used in cardiology to assess the state of blood vessels, but then its methods began to be applied in other areas.
Interventional radiology methods are widely used in gastroenterology, which makes it possible to detect a huge number of diseases in time. With the help of interventional gastroenterology, any patient can perform gastroscopy or detection of formations or polyps, take a biopsy of pathological tissues. This allows you to quickly make the correct diagnosis and start the necessary treatment. To date, the range of manipulations carried out has grown. The volume of interventions has also been expanded.
Interventional radiology in the treatment of esophageal achalasia
Endoscopic transfusion myotomy for esophageal achalasia was first started in Greece, with successful results. The procedure is performed through the mouth using an endoscope in the endoscopy unit. A special scalpel is attached to the endoscope and, with precise movements, cuts the contracted circular muscle fibers in the lower third of the esophagus, which are responsible for the appearance of achalasia. Achalasia is the most common benign primary motor disorder of the esophagus, characterized by poor digestion, regurgitation of undigested food, heartburn and pain, and progressive weight loss in later stages.
Common treatments include esophageal dilatation with an endoscopic balloon and Heller's mitotomy, which occurs in very severe cases, has a high recurrence rate, and is associated with gastroesophageal reflux disease.
The revolutionary oral endoscopic myotomy is the most modern, minimally invasive method of radical treatment of all types of esophageal achalasia. Oral endoscopic myotomy can be performed safely and successfully even in older or critically ill patients. After surgery, patients have no abdominal incisions. Patients can start taking liquid food. The operation helps patients get rid of the daily food nightmare that has lasted for decades in some patients and allows them to enjoy a better quality of life.
Interventional radiology in the treatment of Zenker's diverticulum
Zenker's diverticulum is a rare diverticulum located behind the superior cardioesophageal sphincter. This diverticulum can be caused by incomplete relaxation of the esophageal sphincter in combination with the asynchrony of the muscles in this area. They lead to the formation of a small hernia, which eventually becomes a diverticulum. The disease is more common in people over 60 years of age. It can be diagnosed by x-ray examination of the esophagus and requires careful endoscopic examination. Symptoms include persistent coughing, swallowing, weight loss, and development of aspiration pneumonia.
Until recently, treatment was carried out by open surgery, accompanied by prolonged hospitalization and complications. A new, safe and painless endoscopic method is used with excellent results and 48-hour hospitalization, also without external incisions. The excision is performed under general anesthesia. An endoscope, equipped with a special scalpel, is inserted through the upper esophageal sphincter, and the diverticulum is slowly excised (starting from the mucous membrane, and moving towards the muscle layer). Once the excision is complete, the incision is sutured with metal clips to avoid abscesses and bleeding. The patient must not eat anything for 24 hours.
Interventional radiology in the removal of polyps
Polyps vary in size, ranging from a few millimeters to a few centimeters, and can be found anywhere along the digestive tract.
Submucosal lesions are tumors — usually benign but in some cases malignant — that are located within the wall of the digestive tract. In most cases, they are covered with a normal mucous membrane. When an endoscopy specialist discovers a polyp or submucosal lesion, the first thing he considers is how to remove it completely without causing any complications or any future recurrence. The most difficult polyps to treat are those located in the second part of the duodenum. Before removing any polyp or submucosal lesion, follow these steps:
- the endoscopy specialist must have extensive experience and be able to cope with any complications that may arise;
- nurses must have the necessary experience;
- the removed material is examined by a morphologist.
Polyps larger than 1 cm require special endoscopic examination during polyectomy. The injection helps to separate the mucous membrane and submucosa from the muscle layer. This method also provides data to the endoscopy specialist to see if he can remove the lesion. When the base of the polyp rises smoothly and easily, then the polyp can be removed. Infusion can reduce the risk of bleeding and perforation after polypectomy.
Polyps larger than 2 cm can be removed in fragments or using endoscopic submucosal dissection. Submucosal lesions are removed using a different procedure. Initially, the mucous membrane is exposed with a special scalpel, and the affected part is exposed. Then it is separated from the surrounding tissue and removed.
Endoscopic submucosal dissection
This technique was first developed in Japan to remove an entire large polyp in a single session. This technique reduces the risk of recurrence compared to fragmented polypectomy.
However, it has been proven that endoscopic removal of polyps or submucosal lesions of the digestive tract is a safe method with less risk of complications, especially when specialized endoscopy centers have experienced endoscopy specialists with some training.
Pancreatic pseudocysts
Pseudocysts account for 75% of cystic lesions in the pancreas. They are localized collections of pancreatic enzyme-rich fluid found around the pancreas. These cysts are separated from the fibrous and granulation wall. Pseudocysts are created after pancreatitis or trauma that damages the pancreatic duct and leaks pancreatic fluid. Symptoms of pseudocysts include epigastric pain, nausea, vomiting, and weight loss. In the past few years, pseudocysts have been removed endoscopically. The cyst is detected by ultrasound. A tunnel is created between the stomach and the cyst, and then a special metal stent is placed. Thus, the contents of the cyst are drained into the stomach. The procedure is bloodless, has a low complication rate and other benefits.
These procedures are only a small part of the total volume of operations that can be performed endoscopically. Interventional gastroenterology is constantly evolving and improving.
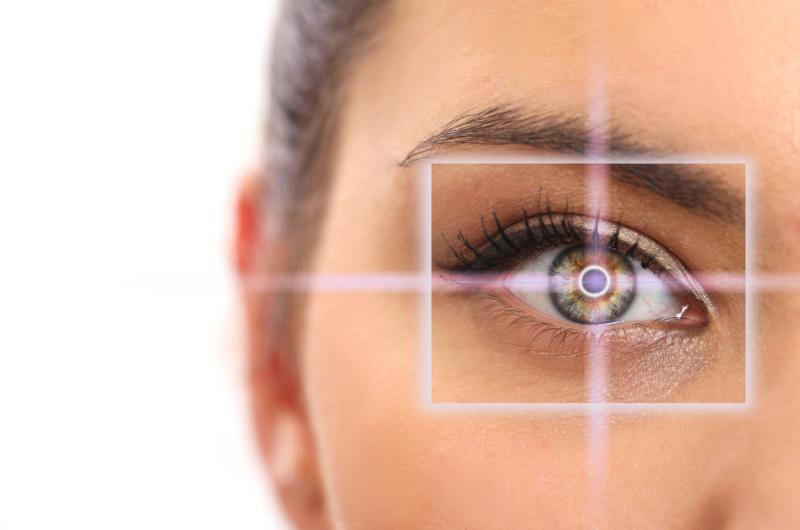
Endoscopic ultrasound (endoscopy, endosonography) is a unique method in which intraluminal scanning of the walls of the studied organ of the gastrointestinal tract is carried out. Also, during the diagnosis, you can study the condition of all adjacent anatomical structures and tissues. An examination is performed using a special echo endoscope, at the end of which a tiny ultrasound probe and an optical instrument are located. Deep penetration of ultrasound into tissues is provided by very high frequencies. Thanks to this, doctor receives images in high resolution, which is impossible with other examination methods.
Today, endoscopic ultrasound of the stomach, pancreas, rectum and colon, the walls of the esophagus, bile ducts, gall bladder and liver is possible. Organs of the mediastinum, lymph nodes located in the chest and abdominal cavities can also be studied.
The main advantages of the technique include:
Capabilities to identify all hollow organ anomalies
Comprehensive study of even "blind" areas
Revealing the exact location of even small growths
Possibilities for biopsy, puncture, anastomosis
Relief of patient's condition (elimination of severe pain) with celiac plexus neurolysis (in the presence of inoperable tumors)
Indications:
The main indications for ultrasound scan (endoscopy) are:
Malignant formations in the esophagus, stomach and colon. Diagnostics is the only method for visualizing individual layers of organs. In early cancer, the procedure allows you to accurately determine the possibilities for removing the tumor by endoscopic interventions. This is due to the fact that during the procedure, doctor receives information about the exact depth of invasion and changes in the lymph nodes. Also, the method can be used to assess the effectiveness of the therapy.
Submucosal formations of the stomach, esophagus and duodenum. Within the framework of diagnostics, it is possible to determine the layer of the wall of a certain organ, from which the formation proceeds, its size and direction of growth. A number of characteristics suggest the histological structure of the tumor. The data obtained during the examination make it possible to determine the tactics of managing patient. If necessary, an endoscopic operation is performed to remove the detected formation. Such interventions do not take long, are relatively safe, but effective. Low-traumatic procedures do not require long-term rehabilitation of patient.
Pancreatic pathology. Endoscopy makes it possible to visualize tumors of even very small sizes (up to 3 centimeters), which are invisible with a standard ultrasound examination. The method allows more accurately than angiography to determine the invasion of the formation into the vascular structures. This is especially important when assessing the forthcoming surgery. Also, the technique is relevant when making diagnoses of acute and chronic pancreatitis. It allows you to distinguish tumor from inflammatory processes and is indispensable in case of an unclear clinical picture. In addition, diagnostics are prescribed to differentiate cysts and cystic neoplasias.
Pathology of the gallbladder and biliary tract. As part of an endo-ultrasound, doctor can detect adenomyosis, polyps, calculi, inflammatory changes, tumors and benign narrowings.
The method is especially relevant for the detection of various lesions of the Vater papilla, bile and pancreatic ducts. This is due to the fact that these areas are inaccessible for visualization when carrying out other diagnostics, while neoplasms are found in them quite often.
How to prepare for the examination?
Proper preparation for endoscopy of the stomach, intestines and other internal organs ensures accurate diagnosis.
A week before the examination, you should exclude from the diet foods that contribute to bloating. Such products include: flour products, cabbage and legumes
Eating and drinking liquids is prohibited 8 hours before the procedure. This is due to the peculiarities of visualization of organs, and the fact that in some cases, during examination, patients experience nausea and vomiting.
On the day of diagnosis, you should stop smoking, which provokes profuse salivation
A few days before the examination, patient takes urine and blood tests. This makes it possible to exclude the presence of contraindications to the procedure and to assess the general state of health. Also, a consultation with the attending physician is prescribed. He interviews patient, makes sure that there are indications for examination, collects an additional anamnesis, which allows him to quickly make an accurate diagnosis in the future.
How is the procedure carried out?
First, patient is positioned on his left side, bending his knees and pressing them to his stomach. Then a special probe is inserted into patient's oral cavity. It moves to the desired organs and, thanks to modern optics, allows doctor to see all the changes. If neoplasms are detected, a tissue biopsy is performed. If necessary, the diagnosis is carried out using pain relievers or under anesthesia. This reduces pain and discomfort.
After an endo-ultrasound, patient may complain of nausea, vomiting, and flatulence. With the correct diagnosis, the discomfort disappears within a few hours.
Contraindications:
Ultrasound endoscopy has a minimal number of contraindications.
Exacerbation of chronic diseases of the gastrointestinal tract
Serious pathologies of internal organs
Relative contraindications can also be identified, in which the examination must be postponed for a while. These include exacerbations of chronic diseases, increased body temperature, general poor health of the patient.
During oral endoscopic myotomy procedure, endoscope is inserted into the esophagus, where an incision is made in the lining of the esophagus. A special knife at the tip of the endoscope is used to cut and create a tunnel in the submucosa of the esophagus. This opens up access to the muscle layer of the esophagus. Next, a myotomy is performed. An endoscopic knife is used to cut and partially remove the inner circular muscle layer from the esophageal sphincter region and the upper stomach. In this case, the sphincter expands, which causes the normal passage of food from the esophagus to the stomach. At the end of the procedure, the incisions are endoscopically clamped and the endoscope removed.
At the beginning of the procedure, the esophagus is irrigated with an antibiotic solution and its maximum cleansing. Then the submucosal cardia is injected at positions from 2 to 3 o'clock. Injections are given approximately 10 cm from the proximal cardiac sphincter. Then, using an endoscopic knife, an incision is made in the mucosa and an entrance to the submucosa. After which dilatation, the balloon is carefully inserted into the submucosal area and dilatation is performed up to 12 mm to initiate the formation of a submucosal tunnel. The endoscope is inserted into the created tunnel and, using a triangular-shaped knife. A careful dissection is performed between the longitudinal fibers until reaching the circular fibers of the esophagus. After that, the circular fibers of the esophageal cardia are dissected, up to reaching the peritoneal tissue, as seen in the video. The cut edges of the muscle are also visible.
After completing the procedure and checking the degree of disclosure of the cardia, the endoscope is removed. At the end of the procedure, clips are placed on the incisions using an endoscope.
A simpler and faster method is spiral enteroscopy. The endoscope is advanced by rotation. The procedure is performed under general anesthesia and lasts 45 minutes.
Spiral enteroscopy uses the transformation of a rotational force into a linear force, thus "collecting" the small intestine on the enteroscope. This procedure is usually performed in pairs, with an assistant rotating the sheath while the endoscopist monitors the progress of the enteroscope through the lumen of the small intestine throughout the procedure. Before performing the procedure, lubricant is introduced into the tube channel. The introduction of the enteroscope begins after carefully fixing the coupling sleeve at the proximal end of the tube at a mark of 140 cm. The device is inserted through the mouth and gently pushed and rotated to the Treitz's ligament, after which the enteroscope is rotated clockwise until the maximum depth is reached. After that, with the help of a special technique, the enteroscope returns to its previous position. This intervention is usually repeated 3 times. The device is removed by turning it clockwise. This procedure requires complete control of patient, therefore deep sedation or general anesthesia is always used. Spiral enteroscopy usually takes less time than balloon enteroscopy. It also allows the enteroscope to be withdrawn and reinserted as needed, while the coiled sheath of the device remains fixed in the small intestine.
Indications:
intestinal bleeding;
suspicion of a tumor;
small intestine polyps;
malabsorption syndrome;
Crohn's disease.